What is Cardiac Resynchronisation Therapy (CRT)?
Cardiac Resynchronisation Therapy (CRT) is a remedy of heart failure that cannot be regularly treated with medication. It is known as ventricular dyssynchrony; this condition may result in a deterioration of symptoms, decreased cardiac output, and low quality of life.
CRT is a type of treatment that involves implanting a device to help transmit electrical impulses to the heart, regulating the contraction of the left and right ventricles. This increases the heart's pumping capacity and can result in a dramatic alleviation of symptoms such as fatigue, shortness of breath, and fluid retention.
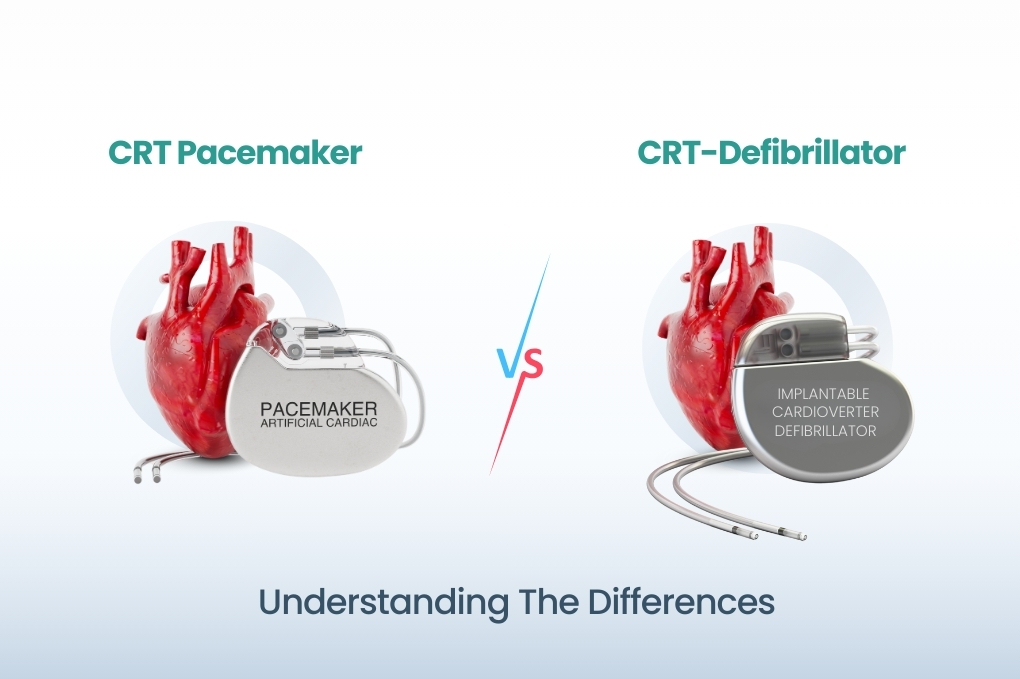
There are two significant forms of CRT devices:
- Cardiac Resynchronisation Therapy Pacemaker (CRT-P)
- CRT-D (Cardiac resynchronisation therapy defibrillator)
CRT-P: Cardiac Resynchronisation Therapy Pacemaker
A CRT-P (CRT pacemaker) is a piece of equipment that applies small electrical charges to both ventricles to regain synchronised heartbeats. It is primarily applicable in cases of mild to severe heart failures, along with electrical conduction disorder,s most notably left bundle branch block (LBBB).
Key Functions:
- Pacing: It activates the heart to pump in a coordinated manner.
- Resynchronisation: It enhances the coordination of heart contractions.
- Symptom relief: Decreases fatigue, elevates exercise tolerance, and improves the quality of life.
- No shock delivery: CRT-P is not able to address potentially life-threatening arrhythmias such as Ventricular tachycardia or fibrillation.
Ideal Candidates:
- Patients having Grade III or IV heart failure (NYHA).
- EF less than or equal to 35 percent.
- QRS prolongation: 130 milliseconds or more (particularly LBBB).
- No past life-threatening arrhythmia.
CRT-D: Cardiac Resynchronisation Therapy Defibrillator
A CRT-D device has all the implants of CRT-P and an in-built defibrillator. This implies that it is also able to identify and cure dangerously rapid heart rates (arrhythmias) by applying an electric shock to rebuild a normal heartbeat.
Key Functions:
- Pacing and resynchronisation: It synchronises the contraction of the ventricles, similar to CRT-P.
- Defibrillation provides life-saving shocks when the heart enters arrhythmias that can be dangerous, such as ventricular tachycardia (VT) or ventricular fibrillation (VF).
- Anti-tachycardia pacing (ATP): Occasional, abnormal rhythms can be terminated without a shock, with fast pacing pulses.
Ideal Candidates:
- Patients with indications for CRT who are in danger of sudden cardiac death related to the presence of dangerous arrhythmias.
- Patients who have a history of cardiac arrest, sustained VT or EF < 50 in the presence of ischemic heart disease.
- This is usually advised for the younger patients, those with limited comorbidities.
Key Differences Between CRT-P and CRT-D
|
Feature |
CRT-P |
CRT-D |
|
Function |
Paces and resynchronizes the heart |
Paces, resynchronizes, and defibrillates |
|
Arrhythmia Treatment |
No |
Yes (VT, VF) |
|
Shock Capability |
No |
Yes |
|
Cost |
Less expensive |
More expensive |
|
Battery Life |
Typically longer |
Shorter due to more functions |
|
Size |
Smaller |
Slightly larger |
|
Implant Procedure |
Less complex |
More complex |
|
Suitability |
Advanced heart failure without arrhythmias |
Heart failure with risk of sudden cardiac death |
Shared Features of CRT-P and CRT-D
Although they are rather different, the following is the list of similarities of CRT-P and CRT-D devices:
Implantation Process: The mode of implantation under the skin (usually in the chest region) is nearly identical.
Leads/Wires: The two devices have three leads, one each in the right atrium, right ventricle, and left ventricle (via the coronary sinus).
Monitoring: Both can record data on heart rhythms, which can be tracked in future examinations.
Symptom Improvement: Both have significant efficacy in improving symptoms and reducing hospitalisation in suitable patients.
How Do Doctors Choose Between CRT-P and CRT-D?
Selection of the CRT-P or CRT-D is based on many factors:
Risk of Sudden Cardiac Death (SCD): CRT-D is a better choice in case a patient is at a high risk of life-threatening arrhythmia.
Age and Life Expectancy: Elderly patients with numerous comorbidities can achieve better results with CRT-P and do not face the risks and complications associated with defibrillator shocks.
Personal Preferences: Some patients may request CRT-P because they are concerned about receiving unnecessary shocks or devices that are too large.
Clinical Guidelines: The majority of cardiologists adhere to international guidelines (like those of ACC/AHA or ESC) in determining the best option.
Risks and Considerations
CRT implants, as well as all medical equipment, are associated with some risks and side effects:
Common Risks:
- Implant-site infection
- Lead dislodgement
- Bleeding, or bearing bruises
- Device malfunction
Specific risk in CRT-D:
- Inappropriate shocks
- Psychological effect of defibrillation
- Seeing that batteries last shorter, one has to replace them more frequently
Regular follow-up and close monitoring with a cardiologist is essential in negotiating such risks.
Life After Implantation
The lifestyle changes and follow-ups are, in general, quite similar irrespective of whether you have a CRT-P or CRT-D device:
Medication Adherence CRT is used as a supplement to medication rather than a substitute for drugs.
Checkups: Regular checkups to monitor the device's battery life and overall performance.
Physical Activity: The majority of patients can return to regular activity, but contact sports should be avoided.
Avoid Magnetic Fields: Avoid strong magnets and inform staff in charge of MRI scans or surgeries.
To Conclude…
Both CRT-P and CRT-D can have a very critical role in the treatment of heart failure, and mainly in patients who have electrocardiographic dyssynchrony. The CRT-P is a complex pacemaker that retimes the heartbeat, enhances heart performance and reduces heart concerns. The CRT-D affords a level of protection in that it addresses life-threatening arrhythmias, which is a possible way of preventing sudden cardiac death.
The decision on the use of either of the two is dependent on the individual's risk coefficients, their history and clinical background, as well as lifestyle choices. This is why they always recommend consulting a licensed cardiologist or electrophysiologist to determine the best course of action for your heart.
The understanding of the distinction between the CRT pacemaker and the CRT-defibrillator enables patients and caregivers to become more involved in treating heart failure and achieve better outcomes.